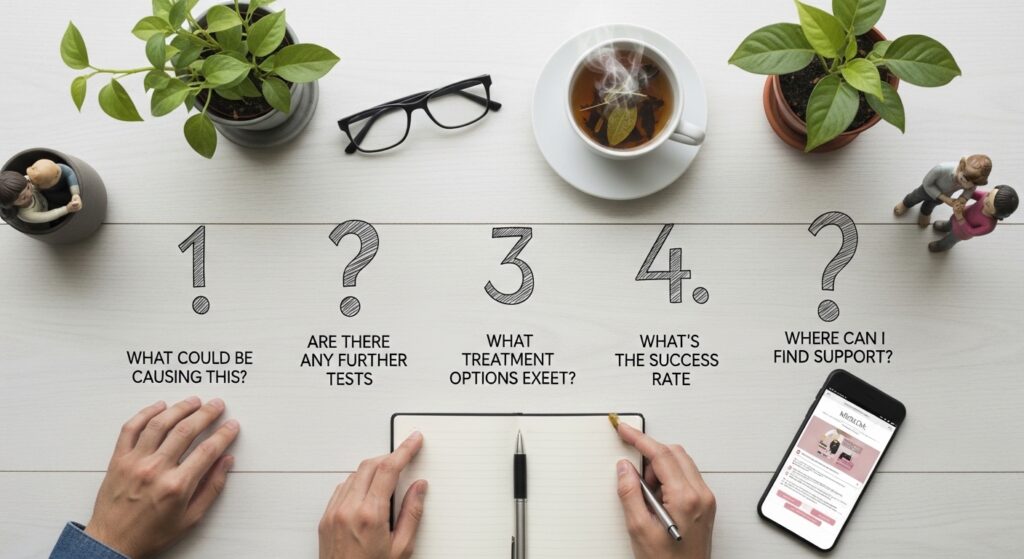
Unexplained infertility is a medical diagnosis that is given when standard fertility tests, such as ovulation assessment and semen analysis, fail to identify a clear cause for difficulty conceiving. Doctors diagnose it after ruling out common reasons such as PCOS, endometriosis, thyroid problems, or sperm problems. This diagnosis may suggest subtle factors such as poor embryo quality or microscopic uterine receptivity issues that lower the possibility of conception. Here are five questions to ask your fertility specialist about an unexplained infertility diagnosis:
1. Which Tests Give More Insight?
Standard fertility testing concentrates on visible reproductive anatomy, ovulation patterns, semen measurements, and general hormone levels. These evaluations are designed to detect major structural or hormonal concerns. Routine screening often excludes detailed evaluation of inflammation inside the uterus and advanced assessment of sperm genetic quality.
Some specialists evaluate markers linked to inflammation in the uterine lining. Some experts evaluate a protein called BCL6 as a possible indicator of irritation or inflammation in uterine tissue. Physicians interpret levels of this protein together with other test results rather than using it alone to make a diagnosis. Advanced imaging, such as ultrasounds, may be used when standard tests, like hysterosalpingograms, leave uncertainty about the shape of the uterine cavity.
An ultrasound performed during the second half of the menstrual cycle provides a more detailed view of the uterine cavity compared with standard imaging. Other tests, such as sperm DNA fragmentation or genetic screening, may be recommended after repeated unsuccessful cycles or pregnancy loss. These tests provide information on subtle egg or sperm issues, helping doctors evaluate the reason behind unexplained infertility.
2. What Are the Odds of Natural Conception?
The probability of conceiving in any given menstrual cycle varies widely among individuals. A fertility specialist evaluates age, cycle regularity, ovarian reserve measurements, overall health, and partner factors to estimate expectations. Clinicians often review hormone and cycle patterns and the results of previous treatments, instead of focusing on just one cycle. Lifestyle patterns such as nutrition, tobacco exposure, alcohol intake, sleep habits, and body weight are reviewed as part of a general health assessment. Doctors examine these factors because they can affect hormone production and ovulation, helping to understand unexplained infertility.
3. What Are the Hidden Causes of Unexplained Infertility?
Some contributors to infertility are difficult to detect through standard testing. Oxidative stress is a process in which unstable oxygen molecules can affect cells, including eggs and sperm. Doctors review the possible effects of oxidative stress on reproductive cells when evaluating fertility.
Changes in uterine blood flow, scar tissue, or prior inflammation may affect embryo implantation. These conditions sometimes require specialized imaging or surgical assessment. Systemic health conditions, including autoimmune or digestive disorders such as untreated celiac disease, are evaluated when symptoms or medical history suggest relevance.
4. What Treatments Might Help?
Treatment plans are individualized and typically progress from less invasive to more advanced options. Doctors often begin with medications that support ovulation. These medications can be used alone or combined with intrauterine insemination (IUI), a procedure in which prepared sperm is placed directly into the uterus around ovulation.
When uterine inflammation or endometriosis is suspected based on symptoms or test results, doctors discuss medication or surgical evaluation. In vitro fertilization (IVF) may be an option when other approaches do not result in pregnancy or when timing is a key factor. Nutritional guidance and lifestyle adjustments are provided as part of comprehensive care.
5. How Is Progress Checked?
Hormone measurements record levels of estrogen, progesterone, and other reproductive hormones throughout the cycle. Ultrasound imaging provides visual information about ovarian follicles and the uterine lining. It also allows doctors to observe overall reproductive anatomy. Cycle tracking records the timing of ovulation and the fertile period. Repeat sperm analyses provide information about sperm count, motility, and DNA characteristics. Pregnancy tests and early ultrasounds help detect when an embryo implants in the uterus and how early development is progressing. By using these tests, doctors will monitor and track changes during infertility treatment, especially when the cause of infertility is unexplained.
Consult With a Fertility Specialist
Advanced diagnostic tests provide additional information when standard testing has not identified the cause of unexplained infertility. Specialized evaluations can reveal inflammation, structural concerns, or timing differences that may influence conception. Specialists use patterns from these tests to identify subtle factors that may affect fertility. Consult a fertility expert to undergo advanced testing and discuss next steps in care.